The adult trigger finger (called, for the thumb, trigger thumb) is a disease characterized by a painful catching and then blockade of the finger in flexion. Frequently the patient cannot straighten the finger without the help of the other hand. In milder forms, the patient presents pain in the palm, at the base of the finger, or dorsally at the proximal interphalangeal joint. In the severe stage, the patient cannot fully straighten his or her finger, even passively, even with the help of the other hand. All fingers may be involved, but the disease most frequently concerns the ring finger and thumb. Sometimes several fingers are affected simultaneously – or at different moments of the patient’s life. People with diabetes are particularly affected. The association in the same patient with trigger finger – carpal tunnel syndrome is relatively frequent.
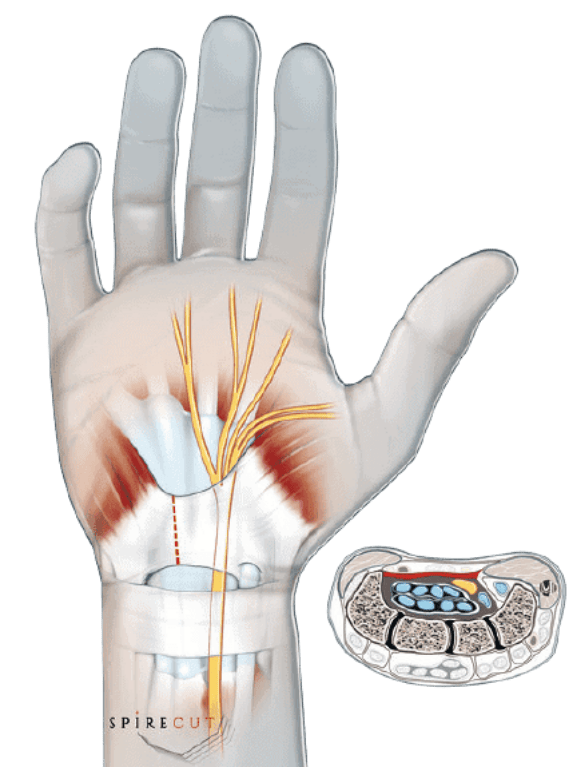
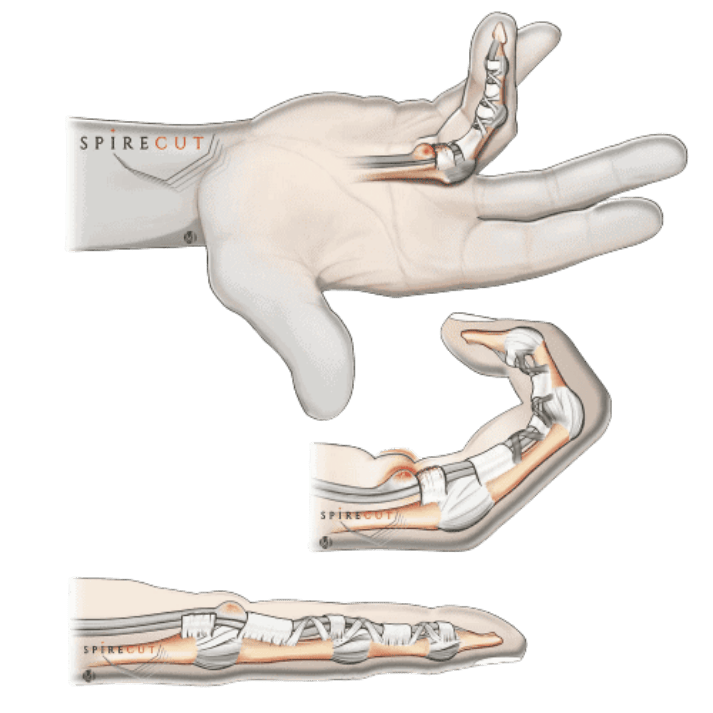
In most cases, the trigger finger is related to the flexor tendon sheath’s thickening, particularly its proximal annular reinforcement called the A1 pulley (several other pulleys). The role of the reinforced sheath is to maintain the flexor tendon(s) (that bend the finger) close to the finger bones. The gliding of the flexor tendon(s) is impaired, and over time erosions may be seen on their surface. The clinical diagnosis is relatively obvious, though experienced hand surgeons know other conditions also causing triggering phenomena. If needed, high-frequency sonography (echography) is used to confirm the diagnosis, usually demonstrating a thickened A1 annular pulley and impaired tendon gliding (dynamic evaluation).
A corticosteroid injection improves many patients, but the affection tends to recur some time after the infiltration. Surgical treatment is then offered, usually consisting of the thickened pulley section, suppressing the tendon’s impingement(s) in the flexor tendon sheath. A small incision does this in the palm. Though successful in most patients, there are complications: the surgical scar can be painful, or the finger may remain swollen for a long time after the operation; some patients present despite the operation with a persistent limitation of finger extension; serious complications are occasionally seen (infection, lesion of a digital nerve). After the operation, most patients cannot return to their daily and operational activities for two or more weeks. Spirecut has developed an original technique and a new surgical instrument (Sono-Instrument) to section the A1 annular pulley without a skin incision under sonography. The patient can return to all his/her activities the next day, including washing the operated hand.
Trigger fingers are also seen in young children, but the condition is quite different – though the surgical treatment is similar. However, the Spirecut trigger finger Sono-Instrument is not designed to be used in a young child.